Unless you’ve been under a very large rock for the last few weeks, you’ve probably caught wind of a wee little virus that’s been making very, very big news. Since first being identified in the Chinese city of Wuhan, cases of a particular strain of coronavirus—now named COVID-19—have been documented on 4 continents. COVID-19 causes a pneumonia-like respiratory illness that ranges from mild to severe. Because it is a very new virus, we continue to learn more as it is being studied.
Is This a Big Deal?
Kind of, yes. The World Health Organization (WHO) has declared it a Global Health Emergency, while the United States has also declared it a Public Health Emergency. China has reported tens of thousands of cases, and ever since it was confirmed that the illness can be spread from person to person, there has been widespread travel restrictions and quarantine measures put in place targeting those suspected to have traveled to or had contact with others who have traveled to endemic areas.
On its surface, this is just another flu-like illness. But one of the biggest reasons that it has caused such widespread panic is that it has just topped over 1000 deaths (as of the writing of this post) and it is still poorly understood. Another reason for so much concern is that the incubation period—the time between exposure and the beginning of symptoms—is a full two weeks, which is a lot of time for someone to be walking around and unknowingly spreading the disease to others. For reference, the incubation period for most colds and flu is only 1 to 4 days.
How Does it Spread?
Much like other respiratory illnesses, COVID-19 is spread from person to person via respiratory droplets. Basically, when people cough or sneeze, their respiratory droplets carry the virus through the air. These droplets either come into contact with others directly or land on surfaces and spread by touch.
What’s Actually True?
Just like anything else that causes widespread panic, there are an awful lot of mistruths and misconceptions spreading about COVID-19.
First, the virus has absolutely nothing to do with beer…I wish I was joking but this seems to be an actual thing going around the interwebs. Second, you shouldn’t be an asshat to anyone because you think they’re carrying the virus. I literally had 2 people come into the ED during a recent shift who thought they had been infected with the virus because they saw an Asian person on their plane. Not joking. I like to think the best of humanity but sometimes people can be awful.
Buzzfeed has a great ongoing story concerning some of the craziest (and even not-so-crazy) disinformation about COVID-19 that is out there at the moment. Basically, don’t believe anything you hear unless it’s from a trusted source, like the CDC or WHO. The WHO also has a wonderful page addressing some of the more common misconceptions about the virus.
Bottom line, don’t believe anything unless it’s coming from a reputable channel and cites information coming from official health sources like the WHO or CDC.
Should I Panic?
Please don’t! However, do make sure you’re doing everything you can to keep yourself and your family healthy. There is so much we don’t know yet about the nature of COVID-19 and how many cases there actually are. And, much like the flu, those most at risk of serious complications are the very young, very old, pregnant women, and those with co-morbid health conditions or immunosuppressed states.
How Can I Protect Myself?
Obviously, if you’ve either traveled to China recently or have been in close contact with someone who has, you should see your doctor immediately. Most institutions (mine included) have implemented protocols for handling patients with risk factors for COVID-19 in a safe and effective manner. We want to take care of you!
Also, winter months often mean we’re cooped up inside in close proximity to others—make sure you’re covering your mouth and nose if you cough or sneeze, WASH YOUR HANDS frequently, and encourage others to do the same. If you have respiratory symptoms, it’s not a terrible idea to wear a surgical mask if you’re going to be around crowds of people to keep from spreading anything to others (like if you have to be out grocery shopping or something). You can also boost natural immunity by making sure you’re eating well, sleeping enough, and getting regular exercise…you know, things we should be doing anyway 😉
It’s true that researchers are rapidly working on a vaccine, but even if there is something that is found to be effective, there is no guarantee that it will be either a) widely available, or b) affordable to most people, so don’t depend on this as a viable option for protection.
How Would I Know if I Was Infected?
Honestly, if you haven’t been to China recently or around others who have, odds are probably pretty slim given strict quarantine measures in place. But this is tough—again, the incubation period is long and the symptoms are really non-specific, especially given that we’re smack in the middle of flu season. It’s impossible to know how many undiagnosed cases there may have been that may have spread beyond the areas where cases are documented.
The symptoms of COVID-19 are very similar to most viral respiratory illnesses and include fever, cough, shortness of breath, and generally feeling shitty. If you have any of these symptoms, please contact your physician.
Is There a Treatment?
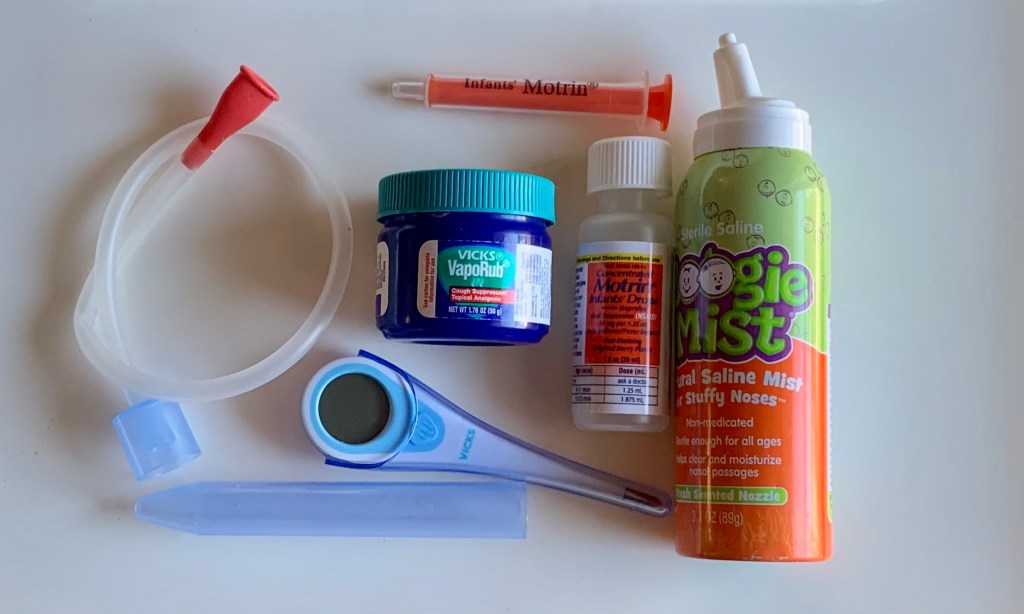
Not really. Again, like the flu or any other viral illness, treatment is supportive—there is no “cure,” just things we do for patients that help manage symptoms. These include things like administering fluids, giving medication for fever and pain, and offering management for cough or trouble breathing. Other than that, the disease has to run its course. The vast majority of people do make a full recovery, but there have been many severe cases and, as I mentioned above, over 1000 known deaths from the disease.
For more information, up-to-date news, and the most recent protocols for providers and the general population concerning COVID-19, check out the Centers for Disease Control and World Health Organization Coronavirus pages.
Image by Gerd Altmann from Pixabay